For years, Community Medical Services has encountered a common problem at all of our clinics: The required starting dose of methadone (30 mg) to treat opioid withdrawal just isn’t enough for many patients.
Methadone is a powerful part of medication-assisted treatment programs (MATs). It blocks receptors in the brain that opioids typically latch onto, easing withdrawal symptoms and preventing cravings. This crucial medicine allows people to resume everyday life while focusing on their treatment. But if patients don’t receive enough methadone, withdrawal can set in, and the whole process of addiction starts over again.
Even worse, patients who don’t get enough methadone to halt withdrawal may continue to use illicit opioids to reduce their symptoms. This significantly puts patients at risk of overdosing.
At Community Medical Services, our main goals are to help patients “stay alive – and thrive.” To do so, we must decrease barriers to getting into and staying in treatment. Most clients need doses much higher than 30 mg – so why do we always start so low?
In this case study, we explore the current landscape of methadone dosing and how it impacts the patient recovery process, share our findings on what higher initial methadone increases achieve, and recommend a better way forward for the healthcare professionals striving to help patients conquer their addiction and reclaim their lives.
Why is the Initial Methadone Dose 30 Mg?
We’ll start with the big question: How did we get here?
The Substance Abuse and Mental Health Services Administration’s (SAMHSA) regulations specifically require that the initial dose on the first day of treatment not exceed 30 mg. Another dose of 10 mg may be given after 2 hours if the patient still has withdrawal symptoms. In no case is a care provider allowed to provide more than 40 mg on the first day. In our experience, few patients want to wait around for 2 hours for only 10 mg more methadone, and the total dose on day 1 is usually 30 mg.
This regulation has been in place for decades, and SAMHSA has been clear that it is serious about this limit. SAMHSA likely chose 30 mg because it is safe for people with no opioid tolerance and unlikely to cause an overdose, no matter what the patient has been using lately.
People who use opioids every day will develop tolerance for them. This means that they will need higher doses to experience the same effects and can tolerate higher doses without becoming sedated or overdosing. It is important to establish a dose of methadone for each patient that matches their own tolerance. However, it is possible to overdose on methadone alone. A dose of methadone that may be too low for one person could be enough to cause an overdose in another.
The Problem with 30 Mg Doses
Some people may do fine at 30 mg or even lower doses; however, some patients need five to 10 times this dose to make it to their next dose with no withdrawal symptoms. If a patient needs 100 mg or more to stave off withdrawals, 30 mg is only going to help them a little. They will still have withdrawal symptoms, especially later in the evening when the methadone is wearing off. When patients continue to have withdrawal symptoms day after day while still coming to the clinic for treatment, they may continue to use other opioids to stave off withdrawal or even get discouraged and give up.
The problem is that we can’t initially tell how much someone will need. One reason for the difference in dose is that people have different tolerance levels when admitted. Their tolerance can depend on several factors, such as what they have been using, how much they have been using, how long they’ve been using, and the route of administration. People also absorb, distribute, and metabolize methadone at widely different rates.
For example, the average dose among all our clinics is currently around 112 mg, but we also have some patients on less than 10 mg and a few on more than 400 mg per day. No two patients are the same, and their treatment needs to be personalized to fit their unique needs. By locking the initial methadone dose at 30 mg, some patients are unable to get the amount of medication they desperately need in a timely manner.
Current Dosage Schedules Are Too Slow
It’s clear why limiting initial methadone doses to 30 mg can be a problem for many patients. But what about after the first day of treatment?
Unfortunately, there is little data to inform us about how fast methadone should be increased. Some studies show that for the first two weeks after starting methadone, the risk of an overdose goes up above what existed before the patient began. After the first two weeks, this increased risk rapidly drops, and as long as patients stay in treatment, their risk of overdosing is 50-70% less than before. However, due to concerns over the possibility of methadone causing an overdose, expert panels and SAMHSA guidelines recommend not only starting at no more than 30 mg but also being careful about dose increases in the first weeks of treatment. According to their advice, the maximum dose for a patient after two weeks of treatment would be 50 mg.
This is not nearly enough for many patients.
SAMHSA assumed that slow titration of the methadone dose would decrease the risk of an overdose in the first one to two weeks. However, this has never been proven.
Why Getting the Dosage Right is Important
We want everyone’s dose of methadone to keep them out of withdrawal until they get their next dose while not causing excess drowsiness. When at the correct dose, people on methadone are ordinary in all respects. If you passed them on the street, you wouldn’t even be able to tell they were on methadone.
However, if the dose is too high, it can cause people to be sedated, slur words, nod off, or be unsteady on their feet. If this starts to happen and the dose isn’t lowered, eventually, people can overdose on methadone.
If the dose is too low, withdrawal symptoms and cravings will return quickly. Patients may seek opioids elsewhere to relieve their symptoms. Or patients may feel like they’re making no progress in their treatment and stop going to the clinic.
There’s a happy medium to be found in correctly dosing a patient with methadone. Community Medical Services believes every patient deserves the chance to overcome their addiction. Delivering the proper medication for every patient is crucial to treatment success.
The Effect of Higher Titration on Treatment Retention Rate
The doctors and care staff at Community Medical Services firmly believe that increased flexibility with the dosage and titration schedule of patients will lead to better outcomes.
To test this, we gathered treatment data from our clinics from the past six years. We wanted to analyze the retention rate of patients in our treatment programs based on how quickly we increased the dosage of methadone to meet their needs.
We reported the average dosage level after a patient successfully completes a seven-day course of dose titration relative to the average percentage of patients who remained in our treatment program for a full 30 days (denoted by Treatment Continuance 30, or TC30).
The graph below includes only patients who started on methadone at 30 mg or less (to exclude transfers from outside programs) and covers the period from 2017 until Q3 of 2023. This analysis uses the 30-day Treatment Continuance (TC30, requiring three out of four doses and at least one dose in the last week of the first 30 days) as the retention measure. The graph shows how the TC30 is affected by the 7-day dose, only including those patients who dosed daily for the first week.
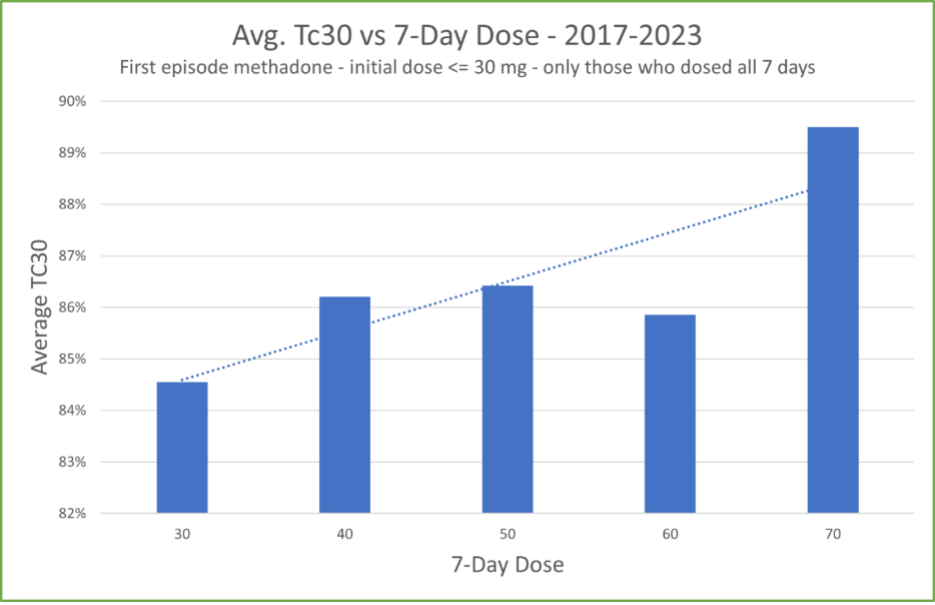
As the graph shows, our hypothesis was correct. Our patients who increased their dosage faster during a 7-day treatment period stayed in the treatment program for 30 days at higher rates than patients who remained at lower dosages.
What Does This Mean?
Community Medical Services is committed to providing the most effective care for our patients, which means doing what we can to improve overall retention.
Medical providers need to be aware that faster titration of methadone to meet a patient’s needs can be the difference between a patient receiving the care they need or dropping out of treatment and continuing illicit drug use. Safely increasing doses faster is a better way to meet patients’ immediate treatment needs and help keep them on the road to recovery longer, increasing the chances of overcoming opioid use disorder (OUD).
As members of the medical community, we also all need to make sure patients are seen after the first week in case they need more dosage increases. Patients who miss dosing during the first week are at high risk of dropping out. We should help them with any barriers they may have (transportation, housing, etc.) and encourage them to keep coming, as the longer they stay in treatment, the more benefits they will get. For example, we’ve witnessed patients who stay in treatment are more likely to be employed, have stable housing and family relationships, and are less likely to overdose.
How We Propose Changing Dosage Guidelines
As this study has shown, current dosage guidelines advocated by SAMHSA and other experts may be more harmful to patient treatment than helpful. They impose barriers that may leave patients suffering the most from OUD to fall through the cracks. When done safely through careful triage and monitoring, giving a larger initial dose of methadone to patients suffering from severe dependency and titrating to higher dosages more quickly could decrease the chances of overdoses, reduce the chances of a relapse, and increase the chances that a patient will continue seeking treatment for their condition.
At present, we cannot do anything about initial dosage rates until SAMHSA revises the 30 mg requirement. Fortunately, they have indicated they may be willing to increase initial dosage allowances later this year.
What we, as providers, can control is the rate of increase after the initial methadone dosage. At Community Medical Services, we suggest increasing the dose of methadone much faster than the SAMHSA panel recommendations. We always comply with regulatory requirements – our initial dose is never more than 30 mg for patients starting newly on methadone. However, our guidelines allow for titrating the dose as high as 60-70 mg by day 7 in patients who need higher doses.
Our clinical experience suggests that the SAMHSA recommendations are too conservative. Our medical providers assess each patient, considering their use patterns, and individualize their dosing regimen. In addition, our nurses assess each patient at the dosing window before any dose increase. We believe our patients tell the truth and will be open about what they are using and how much if we approach them with a nonjudgmental attitude, and they will let us know if they are experiencing drowsiness or their dose is too high. By working together and listening to our patients, we can be more successful in helping them recover from their addiction.
Over years of using our dose titration protocols, we have not had any significant problems, and we feel we have achieved a better balance between the risk of an overdose and the risk of dropping out of treatment.
Mitigating Risks
The concerns about increasing methadone dosages too rapidly are not unfounded. Methadone, like any major medication, can result in overdosing if not used correctly. However, Community Medical Services has established strategies to ensure the safety of patients while giving them the treatment that best meets their needs.
It is important that we talk with our patients at intake about overdosing, the risks of using other opioids on top of methadone, and how to decrease their overdose risk (not using alone, using a test dose, having a naloxone kit around, etc.). Our nurses assess each patient at the window. If the patient is sedated or reports that their dose is too strong, the medical provider is notified, and the dose is adjusted accordingly. Patients who have not been using a lot of opioids recently (coming out of incarceration or an abstinence-based treatment program or a self-imposed taper at home) are started and induced on lower doses. However, in our experience, the majority of the patients that come to us require higher doses.
Making Methadone Treatments Safer Together
At Community Medical Services, the safety and health of the patient is our biggest concern. We firmly believe that with the proper ability to match methadone doses to a patient’s unique needs, we can safely and effectively set them on the right course for recovery from their substance use disorder.
We’ve built safety standards to ensure patients are accurately matched to the correct initial dose when they visit our clinic for the first time. Then, we monitor them as they’re titrated to the proper dosage at the beginning of their treatment to give them the best chance of success for recovery.
As healthcare professionals, we have an opportunity to significantly improve the lives of our patients struggling with opioid addiction. The data shown above suggests that the current dosage guidelines from SAMHSA don’t work for many patients. Low initial doses and titration scales put patients who have severe OUD at risk of leaving treatment.
Some groups are working on improving the current methadone induction standards – providing research data or developing new technologies (such as point-of-care methadone levels or wearable devices to detect impending overdoses). Our hope is that these efforts, working together with the regulators at SAMHSA, will move our treatment forward and help more people who are suffering from opioid addiction.
New regulations were released by SAMHSA that will take effect on April 1, 2024. These regulations implement some of the changes recommended in this blog, including increasing the initial allowed methadone dose from 30 to 50 mg. It is still a challenge to get patients to a therapeutic dose as rapidly and safely as possible, and more needs to be done to make this a possibility for all patients.









