The Impact of Urine Drug Screens on Patient Retention and Social Outcomes at CMS

Urine drug screens (UDSs) are used in opioid treatment programs to help clinicians track patient progress, adjust treatment plans, and address potential risks. At Community Medical Services, we’ve gathered extensive data from UDS results to understand better trends over time and how these results affect other important outcomes, such as patient retention and Social Determinants of Health (SDOH).
With over 2 million documented tests since 2004, our UDS data provides a detailed picture of the substances our patients use and how their use changes throughout treatment. This article explores our key findings, including trends in opioid, fentanyl, and amphetamine use, as well as the connection between drug screen results, retention rates, and social factors like employment and housing.
By analyzing these trends, we can refine our treatment strategies to better support our patients, help them stay in treatment and improve their overall quality of life.
UDS at CMS: What We Test For
As of March 2024, Community Medical Services had over 2.1 million documented urine drug screen tests. These tests provide critical insights into what substances our patients use and help inform treatment plans and strategies. The drugs we routinely test for include:
- Opiates (including heroin, hydrocodone, codeine, and morphine)
- Oxycodone
- Barbiturates
- Benzodiazepines
- Cocaine
- Amphetamines (including methamphetamine)
In response to the growing fentanyl crisis, we more recently added tests for fentanyl and heroin (via the 6-monoacetylmorphine or 6-AM metabolite specific to heroin). Importantly, we do not routinely test for cannabis unless required by state regulations or ordered explicitly by a medical provider. Additionally, CMS tests for the medications we administer, including methadone, methadone metabolites, and buprenorphine.
We conduct most of our testing at our lab in Scottsdale, but some states require external labs. All results are uploaded into our Electronic Health Record (EHR) and transferred to the Data Warehouse, where we conduct our analyses using Databricks. We currently perform close to 100,000 tests each quarter, and this extensive data collection allows us to track trends in substance use and improve the effectiveness of our treatment programs.
Trends in CMS UDS Results
As we analyze UDS data over time, we can observe clear trends in opioid and fentanyl use among our patients. One of the most notable findings is the sharp rise in fentanyl positivity. Fentanyl began appearing in our tests around late 2019, and it has since become one of the most frequently detected substances. By early 2024, over one-third of all tests conducted at CMS were positive for fentanyl. In contrast, the percentage of tests positive for other opiates, such as heroin and prescription opioids, has been steadily declining over the same period.
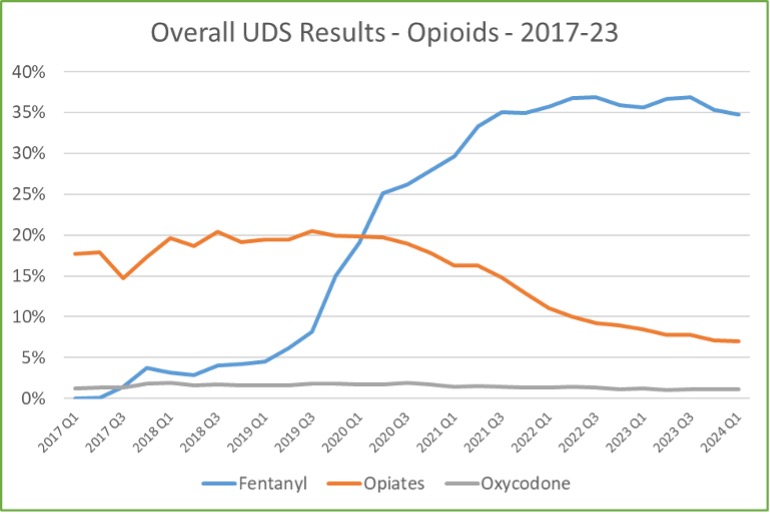
The rate of oxycodone positivity has remained stable, hovering around 1-2%, which is relatively low compared to other opioids. This suggests that while fentanyl has surged in prevalence, the use of other opioids has either stabilized or decreased.
To better understand these trends, it’s important to look at the timing of tests within the patient’s treatment journey. Not all tests focus on newly admitted patients; many of our tests involve individuals who have been in treatment for extended periods. The majority of UDS tests—more than 75%—are conducted on patients who have been in treatment for over two years. The graph below shows the percentage of patients who test positive upon admission for fentanyl, opiates, or oxycodone:
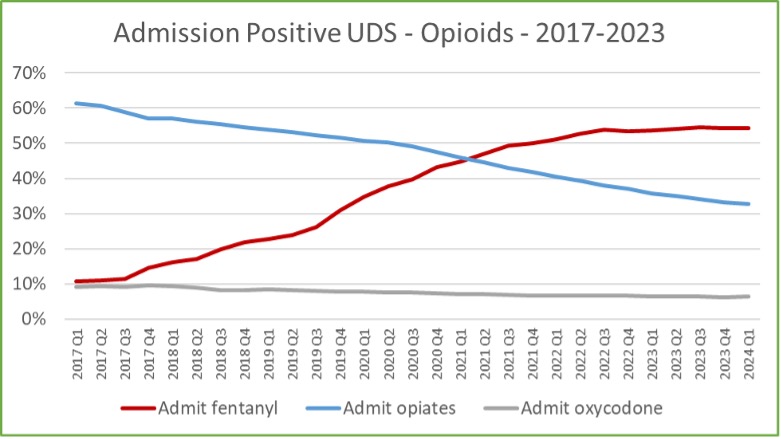
The percentage of opioid positivity on admission shows a similar trend as the overall rate for all tests, with an increase in fentanyl positivity and a decrease in opiates, with a minority of tests positive for oxycodone.
The graph below shows the percentage of patients who test positive at the time of admission for drugs other than opioids – amphetamine, cocaine, and benzodiazepines.
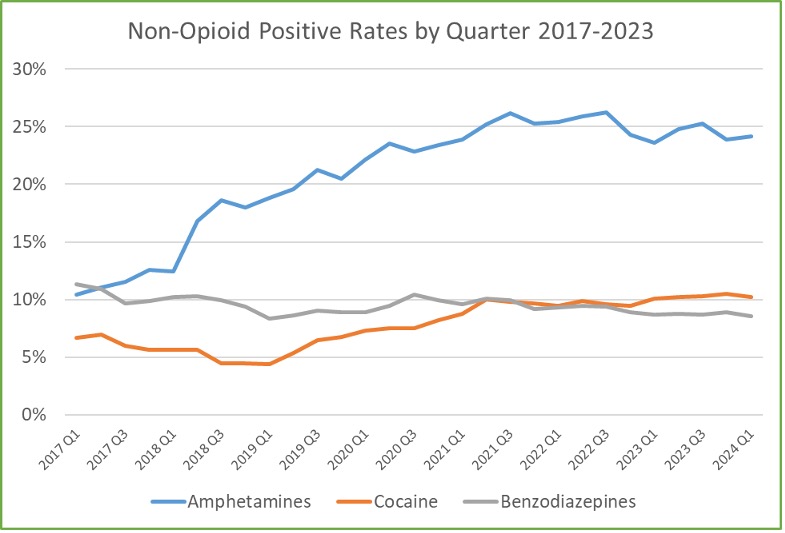
The percentage of patients positive for amphetamine on admission (mostly due to illicit methamphetamine use) has been increasing dramatically over the last few years.
Fentanyl and Amphetamine Positivity Over Time
One of the most concerning trends observed in our UDS data is the persistently high rate of fentanyl and amphetamine positivity, even among patients who have been in treatment for extended periods. While the percentage of positive tests declines as time in treatment increases, a significant number of patients continue to test positive for these substances long after their initial intake. This data provides insights into the long-term challenges patients face, particularly with substances like fentanyl, even after extended time in treatment.
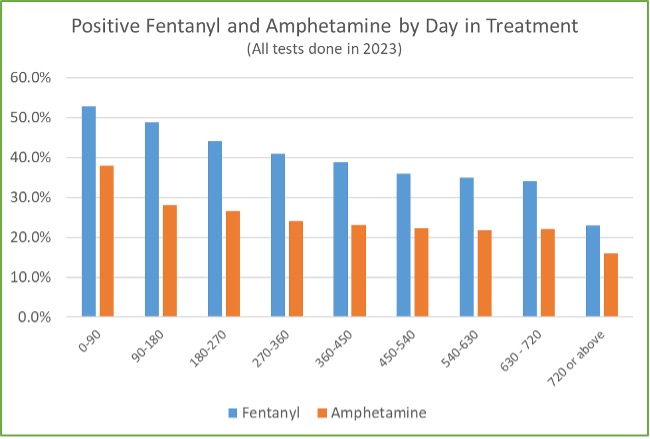
For example, approximately one-fourth of patients who have been in treatment for over two years still test positive for fentanyl. Similarly, about 16% of patients in this group test positive for amphetamines. This data highlights a critical reality: many patients do not become fully abstinent, even after years of treatment. Additional analysis shows that two-thirds of patients who test positive for fentanyl upon admission are still testing positive after one year of treatment.
Despite this ongoing substance use, patients must remain in treatment. The data shows that while complete abstinence may not be achievable for all patients, staying in treatment provides significant health benefits, such as reducing overdose risk and improving overall health and stability. Rather than discharging patients based on UDS results, it’s essential to continue supporting them through treatment, helping them “stay alive and thrive.”
State-Specific UDS Results: Variations in Fentanyl and Amphetamine Positivity
While the overall trends in fentanyl and amphetamine use are alarming, there are significant variations in UDS results depending on the state. This regional variation highlights how the opioid crisis and substance use patterns can differ widely across the country, influencing treatment strategies and outcomes. The following tables show the percentage of positive UDS results on admission for fentanyl and amphetamine across several of the states CMS serves:
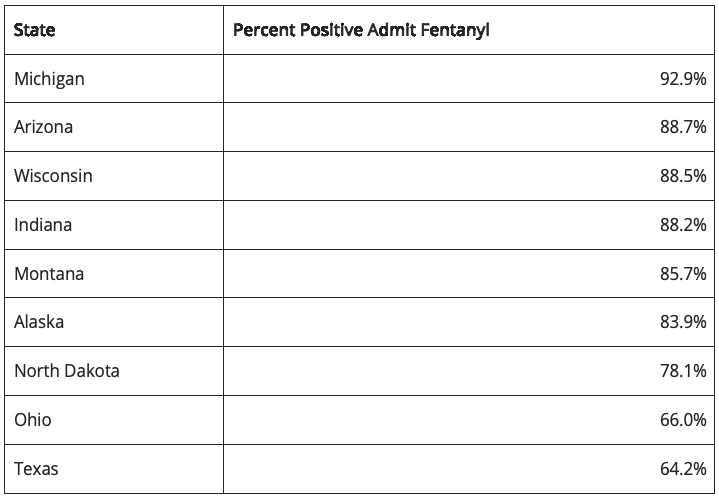

During the first quarter of 2024, Michigan had the highest percentage of fentanyl-positive admissions, with Arizona, Wisconsin, and Indiana also reporting high percentages of fentanyl positivity. In contrast, states like Ohio and Texas showed lower fentanyl positivity rates, though they remain concerning.
Amphetamine use, on the other hand, displays a different regional pattern. Alaska, Montana, and Arizona reported the highest percentages of amphetamine positivity at admission. Conversely, Wisconsin, Michigan, and Ohio showed much lower rates of amphetamine use but exhibited higher rates of cocaine use. These variations in stimulant use suggest that different regions may have distinct substance use trends, which require tailored treatment approaches.
Understanding these state-level variations is crucial for developing targeted treatment plans that address the specific needs of patients based on their region. By identifying these trends, CMS can better allocate resources and customize care strategies to combat the unique challenges faced in each state.
The Impact of UDS Results on Treatment Retention
The connection between urine drug screen results and patient retention in treatment is an important factor for understanding the long-term success of opioid treatment programs. At CMS, we’ve observed that positive UDS results, particularly for fentanyl and amphetamines, have a clear impact on 30-day retention rates.
Patients who test positive for fentanyl at admission have a lower retention rate compared to those who do not. Specifically, the retention rate for fentanyl-positive patients drops from 80% to 70% after 30 days. The effect of amphetamine positivity is even more pronounced: those who test positive for amphetamines at admission have a 30-day retention rate of just 65%. This highlights that amphetamine use presents a significant challenge for patient retention.
Patients who test positive for both fentanyl and amphetamines have a retention rate like those who test positive for amphetamines alone, hovering around 65%. These results suggest that amphetamine use may be a stronger predictor of lower retention than fentanyl alone, indicating that patients using amphetamines face additional challenges in maintaining their engagement with treatment.
These findings underscore the importance of early intervention and continued support for patients who test positive for these substances. While fentanyl and amphetamine use are associated with lower retention, keeping patients in treatment and providing comprehensive care can help mitigate these risks and improve long-term outcomes.
Impact of UDS Results on Social Determinants of Health (SDOH)
In addition to affecting retention, UDS results have a significant relationship with Social Determinants of Health (SDOH), such as employment and housing stability. By analyzing these factors alongside drug test results, we can better understand the broader implications of substance use on patients’ lives.
For patients who test positive for fentanyl upon admission, the data shows little to no impact on their employment or housing status at the time of intake. This is likely because fentanyl use has become so widespread among our patient population. Patients who test negative for fentanyl on admission, while they have not used fentanyl in the prior few days, may still have a history of fentanyl use before that time frame
However, the picture changes when looking at amphetamine use. Patients who test positive for amphetamines on admission are less likely to be employed and more likely to have unstable housing than those who test negative. The data indicates a strong link between methamphetamine use and adverse SDOH outcomes. This is likely due to the specific effects of amphetamine use, which can have a more immediate and disruptive impact on a person’s ability to maintain employment and housing.
These findings highlight the importance of addressing both the substance use disorder and the social challenges that come with it. For patients struggling with amphetamine use, targeted interventions that focus on employment support, housing assistance, and mental health services are essential to improving their overall stability and success in treatment.
Demographic Insights from UDS Results
Beyond substance use trends and their impact on retention and social factors, urine drug screen results also reveal important demographic patterns. At CMS, we’ve analyzed the relationship between UDS results and patient characteristics such as age, gender, employment status, and treatment type, providing valuable insights into how different groups are affected by opioid and stimulant use. This table shows the average admission UDS results for 2023 for fentanyl and amphetamine by demographic factor:
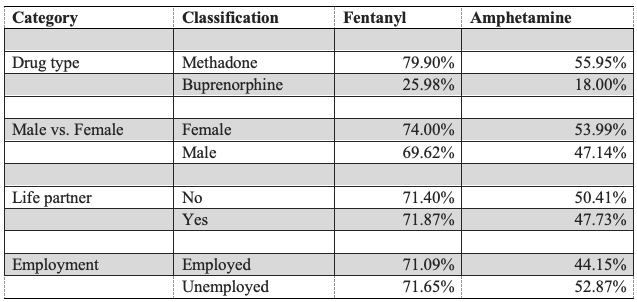
- Fentanyl and Amphetamine Positivity by Treatment Type: One key finding is the difference in UDS results between patients receiving methadone and those receiving buprenorphine. Patients who begin treatment with methadone have much higher rates of fentanyl and amphetamine positivity than those who start with buprenorphine.
- Gender Differences: There are also notable gender differences in UDS results. Females tend to have higher positivity rates for both fentanyl and amphetamines compared to males. These gender differences highlight the need for gender-sensitive approaches in addressing substance use and tailoring treatment plans to meet the unique needs of each group better.
- Employment and UDS Positivity: Employment status also plays a role in UDS results, particularly for amphetamines. While unemployment does not appear to have a significant impact on fentanyl positivity, it is closely associated with higher rates of amphetamine use. This suggests that methamphetamine use may contribute to more difficulty in maintaining employment, reinforcing the need for employment support as part of comprehensive treatment plans.
- Age and Substance Use: Age is another factor that influences UDS results, particularly for fentanyl. The data shows that younger patients, particularly those in the 20-30 age group, are more likely to test positive for fentanyl. In comparison, older patients have a significantly lower positivity rate. Amphetamine use, on the other hand, does not vary much with age.
- Multiple Treatment Episodes: Patients with multiple treatment episodes—those who have been discharged and re-admitted—tend to have higher rates of fentanyl and amphetamine positivity. As the number of treatment episodes increases, so does the likelihood of testing positive for these substances, reflecting the challenges faced by individuals with more complex or prolonged substance use disorders.
How CMS is Improving Treatment with UDS Data
The data we’ve gathered offers valuable insights into the challenges faced by patients in treatment for opioid use disorder, particularly regarding fentanyl and amphetamine use. One of the most important takeaways from our analysis is the need to keep patients in treatment, even if they continue to test positive for substances. The data shows that many patients, especially those who test positive for fentanyl at admission, continue to test positive even after a year or more in treatment. While abstinence may not be achievable for all patients, staying in treatment offers significant benefits, such as reducing the risk of overdose and improving overall health. By accepting that some patients may never entirely abstain from substance use but can still experience improvements in stability and health, we can better support their recovery journey.
The trends and data CMS has collected provide a roadmap for improving treatment outcomes and addressing the complex needs of our patients. From recognizing the importance of keeping patients in treatment despite ongoing substance use to understanding the social and demographic factors that influence recovery, this data shapes the future of opioid treatment programs at CMS.
By focusing on long-term retention, addressing social challenges, and tailoring treatment to specific patient needs, we can continue to progress in helping our patients “stay alive and thrive.” If you or a loved one is looking to start your journey toward recovery, find a CMS clinic near you today.

About the Author
Dr. Robert Sherrick was appointed as CMS’s first Chief Science Officer in 2023, transitioning from Chief Medical Officer, a role he served for years.
Prior to serving CMS he had experience working at an inpatient addiction treatment facility in Montana, Pathways Treatment Center, treating all forms of Substance Use Disorders and dual diagnosis patients. Dr. Sherrick has been providing Medication Assisted Treatment for Opioid Use Disorder since 2003, initially in an office setting using buprenorphine and subsequently with methadone in Opioid Treatment Programs.
He established a state-wide buprenorphine treatment program for VA Montana with an extensive focus on telemedicine. He is board certified in Addiction Medicine through the American Board of Preventative Medicine and is the Immediate Past President of the Northwest Chapter of the American Society of Addiction Medicine.
Dr. Sherrick received his MS and BS degrees in Electrical Engineering from the Massachusetts Institute of Technology, and his MD from George Washington University Medical Center.
Related Content
Why Do We Have Opioids? Medical Benefits, Drawbacks & Misuse
It’s not news to people at this point that we have a major opioid crisis in the United States. Millions of Americans have become addicted to opioids in various forms, causing thousands of deaths from overdoses every year, putting a large strain on our healthcare system, and shattering families with the debilitating symptoms of drug abuse.
Treating Opioid Use Disorder While Pregnant: Addressing Your Concerns While Expecting
Pregnancy can be a special time, full of joy and anticipation. But for women struggling with an addiction to fentanyl or other opioids, it can be difficult and stressful. Every woman wants to be a good mother and do everything she can for her baby, but having to deal with an addiction makes it significantly more challenging.
How Does Methadone Work?
Addiction is a very powerful thing. Opioid addiction is even more so. The opioid addiction epidemic has been sweeping our nation for years now. During this time, medical experts have banded together to devise new and better ways to treat patients suffering from opioid use disorder (OUD). Methadone has long been a tried and true staple in the substance abuse doctor’s trusty toolkit. But how does it work?




